One Million Hospital Admissions A Year Linked To Obesity
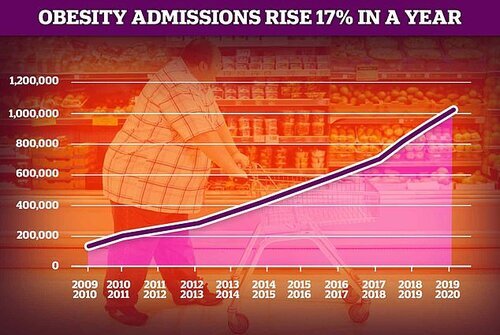
NHS Digital released data this month which shows that obesity is linked to one million hospital admissions in the year between 2019 and 2020. A total of 1.02million hospital admissions had obesity listed as the main or secondary cause for their visit, a rise on the 876,000 the year before.
The NHS figures show that around 10,780 admissions were caused directly by obesity while the rest were for problems related to obesity, a rise of 17% from the previous year. Admissions directly caused by obesity were highest in people aged 45 - 54, lowest in people aged under 16 or over 75 and women made up 64% of cases.
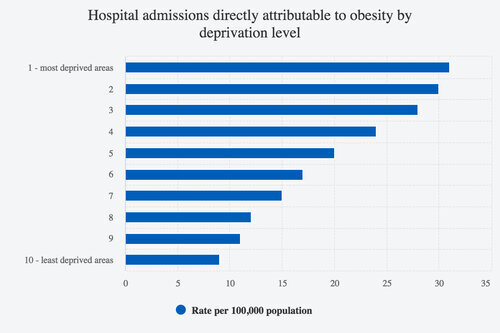
Of the admissions where obesity was a factor but not the main reason for admission, the most common of these were for appointments during pregnancy, knee and hip arthritis and heart disease. Obesity admissions were twice as likely in the most deprived areas of the country compared to the least deprived.
The C-Word
Being obese or excessively overweight increases the risk of severe illness and death from Covid-19, a July 2020 Public Health England report confirms. The current evidence does not suggest that having excess weight increases people’s chances of contracting Covid-19 however, the data does show that obese people are significantly more likely to become seriously ill and be admitted to intensive care compared to those with a healthy BMI.
A study found that people with a BMI of 35 - 40 have an increased risk of death from Covid-19 by 40% and this rises to a 90% increased risk of death when a person has a BMI over 40.
Evidence published both in the UK and internationally suggests that being severely overweight puts people at greater risk of hospitalisation, The risk of intensive care unit admission and death from Covid-19 increases substantially as body mass index (BMI) increases and 7.9% of critically ill patients with Covid-19 had a BMI over 40 in intensive care units, compared with 2.9% of the general population.
This could indicate why countries which have both obesity problems and an ageing population had high death rates attributed to Covid-19. Flipped on its head; the more unhealthy a population, the less unexpected it is when large amounts of unhealthy people die from things that don’t affect those who are healthy or not elderly. This seems to be reflected in the ONS data which published a report showing that 772 people under the age of 65 were recorded as Covid-19 deaths with no underlying health conditions between March and June 2020 (they’ve not continued to update this information to present day).
Do As I Say, Not As I Do
Something that doesn’t go unnoticed but is rarely spoken about is the shockingly high level of obesity within the NHS itself. According to a Royal College of Physicians estimate, 700,000 NHS employees - including 1 in 4 nurses - are obese, yet only 15% are seen or assessed
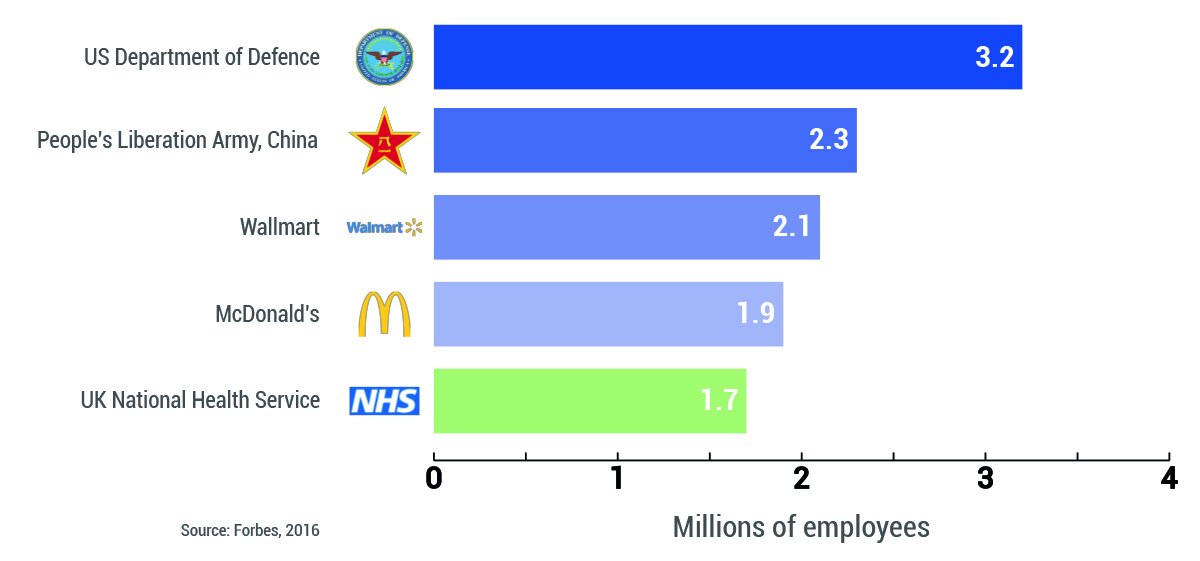
Obesity is recognised as contributing significantly both to illness and employee absence so considering the NHS is the fifth largest employer in the world, this translates into large amounts of money being spent to deal with these issues. A report into health and wellbeing in the NHS suggested that if current rates of sickness were reduced by a third, this would result in an estimated annual direct cost saving of £555 million as well as 3.4 million additional available working days for NHS staff every year.
Primary care trusts (PCTs) are responsible for overseeing area hospitals and ensuring their quality, yet an audit of London PCTs showed that only 8% had specific policies for physical activity, 19% had healthy eating policies and few had policies targeting broad health issues. The authors of the report say that doctors and healthcare staff ‘do not receive adequate training in obesity, healthy eating, physical activity and behaviour change techniques or the prevention of excessive weight gain’ yet, unsurprisingly, the main barriers cited to the creation of proactive wellbeing programmes were lack of funding (a perennial ‘reason’) and lack of time.
Considering the NHS themselves highlight how obesity is linked to heart attacks, diabetes, cancer, strokes, cardiovascular problems, it begs the question - why are they not enacting proactive policies to educate, treat, inform and prevent obesity? After all, an ounce of prevention is worth a pound of cure.
In 2015 McKinsey & Company published a study showing that the UK government currently spends 5% of the entire budget of the NHS every year on the direct medical costs of conditions related to being overweight or obese. The per capita spending on patients increases significantly between people with a normal BMI (<25) and different overweight classes. Between a normal BMI (<25) and overweight (25-29) there is an increase of 31% or £247 per capita. For obese class 1 (30-34) there is an increase of 58% or £469, for obese class 2 (35-39) the increase is 80% or £642 and for the highest weight class, obese class 3 (>40), there is an 86% or £688 increase.
The UK has the second-highest rate of obesity in the world and the largest in Europe, with a quarter of all adults classed as obese with almost two-thirds (63%) of adults in England classed as overweight or obese. In 2018 the majority of adults in England in 2018 were overweight or obese (63%) and it’s estimated that the majority of the population will be classified as obese by 2050.
Annual spend on the treatment of obesity and diabetes is greater than the amount spent on the police, the fire service and the judicial system combined with £48 billion a year spent managing the social causes and healthcare of obesity. Obesity is classed as the biggest strain on the NHS and is a huge financial burden; how ironic considering that the many people who claimed we needed to protect the NHS by simply staying in our houses, haven’t spent as much money or propoganda in highlighting the obesity epidemic which continues, year after year.
A Legend In Our Own Mind
Nothing lasts forever and no matter how powerful, all governments, kingdoms or societies ultimately fall. The Roman Empire’s decline was gradual, probably imperceptible to those living through it. 1920 marked the year the British Empire became the largest Empire in history yet 100 years on, Britain clings on to past glories and still claims to be important and influential on the international stage, unable to come to terms with the loss of power and prestige.
American political scientist Kenneth Waltz created a set of five criteria to determine what defines a great power:
Economic Capability
Military Strength
Resources
Political Stability & Competence
Population & Territory
By these measures, Britain has now dropped out of the premier league of world affairs. It is hard for anybody let alone a nation to accept they’ve passed their peak, however Britain is a shadow of its former self and its decline is visible in terms of ever-reducing material and diplomatic capabilities. Note how tenaciously we cling on to the ‘special relationship’ we have with America, even though Washington is far more interested in Asia than Europe. As far back as 1991, American ambassador to London Raymond Seitz said: “Never forget that the United States is only interested in Britain in so far as Britain is a player in Europe.”
The decline of the West coincides with the rise of the East and the world is moving into a duopoly, with America and China the current great powers, with Russia and India on the ascendancy. Britain slides down the rankings and this relegation to a new, less important and influential role will prove to be exceptionally painful and difficult to accept.
“What experience and history teach us is this - that people and governments never have learned anything from history, or acted on principles deduced from it.”
The decline of an Empire can often be mirrored with the decline of morals and ethics within it, as James Traub writes:
‘In The History of the Decline and Fall of The Roman Empire, Edward Gibbon luridly evokes the Rome of 408 A.D., when the armies of the Goths prepared to descend upon the city. The marks of imperial decadence appeared not only in grotesque displays of public opulence and waste, but also in the collapse of faith in reason and science. …A decadent elite licenses degraded behavior, and a debased public chooses its worst leaders.’
We now find ourselves living in a country whose future is far less certain and ‘glorious’ than its past. Our strong beliefs in self-reliance, resilience, stoicism and self-determination have been replaced with an attitude of expecting something for nothing. Government welfare now supports so much of the country it has come to be seen a natural right for everyone forever. Yet, when so many policies end up making the wrong thing easy and the right thing hard, it shouldn’t be a stretch to imagine that when there are no negative consequences for ignoring you health and no financial costs to pay for your own healthcare, an attitude of entitlement grows unchecked. When healthy people who rarely use a healthcare system are forced to subsidise other people’s healthcare costs in the form of higher and higher taxes then it is only a matter of time before things reach a breaking point.
What holds costs down is patients acting like consumers, looking out for themselves in a competitive market. Providers fight to win business by keeping costs down and quality up…When someone else pays, costs always go up....(and) we consume without thinking.
- John Stossel
Conclusion
If obesity is such a huge burden to our healthcare system (which we have venerated and vowed to protect), and when per capita spending on patients increases significantly between normal BMI and different overweight classes, what are the incentives for people themselves to change their behaviour and make healthier lifestyle choices?
When a significant number of hospital admissions are obesity related, who really is it that’s being reckless and not protecting the NHS with their behaviour?
I have written before (here and here) about the the various aspects of healthcare we rarely like to address. As I also mentioned, I’m not in favour of a radicalised, emotion-driven response to complex issues. It feels satisfying to tie all arguments about the NHS into a bow called ‘it needs more money and it’ll be fixed’, yet this must also be questioned.
Why does it need more money?
Is it due to bad management?
Is an increasingly unhealthy population demanding too much from it?
With an ageing population, and the increasing prevalence of chronic lifestyle-related diseases, if the NHS is going to continue in its current form, it needs to reflect the changing needs of the population it serves. It needs to be proactive promoting health and wellbeing instead of concentrating on recovery after illness. The issues connected to obesity are not going to go away; they are going to compound over time and, instead of deluding ourselves our NHS is the jewel in the crown of a healthcare system envied throughout all the world, we need to be realistic and question if the model is simply unable to cope with the demands of modern-day society which is so different to the world when it was created in 1948.
As would be expected, a declining empire would be matched by a decline in living standards; wage growth is not expanding at a pace that keeps up with the rising cost of living nor the growing costs of healthcare, so where is the ever-increasing NHS budget going to come from?
The NHS is funded mainly from general taxation and this growing gap cannot be plugged indefinitely by raising taxes and treating the British public as cash cows, yet we are acting as if it’s natural to have an unlimited supply of money to deal with the problems obesity causes.
What is shocking is the ease with which we have normalised obesity and accepted it as a part of everyday life; it’s as if, collectively, as a country we’ve metaphorically and physically let ourselves go. However, awareness is the first part of the process; introspection is hard, but we can forge a new identity if we accept our place in the world. To start the transformation, the only pie we need to be eating for the foreseeable future is that of the humble variety.
REFERENCES
Statistics on Obesity, Physical Activity and Diet, England 2021
It’s time to ban obesity in NHS employees
NICE calls for NHS staff to become active to cut obesity
Action on obesity: Comprehensive care for all
Excess weight can increase risk of serious illness and death from Covid-19
Excess weight and COVID-19: insights from new evidence
The NHS is the world’s fifth largest employer
How does UK healthcare spending compare with other countries?
Covid-19 deaths with no underlying health conditions, broken down by age
Davey RC, The obesity epidemic: too much food for thought? British Journal of Sports Medicine 2004;38:360-363.
Health matters: obesity and the food environment
The obesity crisis | McKinsey Study
Can India learn to be a ‘Great Power’?
Mahase E. Covid-19: Why are age and obesity risk factors for serious disease? BMJ 2020; 371 :m4130 doi:10.1136/bmj.m4130
CDC study finds about 78% of people hospitalized for Covid were overweight or obese
A Recessional Power: How Britain’s Claim to Be a Great Power Has Been Fatally Undercut
Just How Special is the U.K.-U.S. ‘Special Relationship’? One Briton’s View
The United States of America Is Decadent and Depraved
Living Standards 2017The past, present and possible future of UK incomes
How the NHS is funded | The King's Fund
Revealed: How the world gets rich – from privatising British public services
UK Sin Taxes Now A ‘Cash Cow’ For Government: Report
Taxman accused of using small businesses as a 'cash cow' after unveiling 'draconian' penalty regime
This is a social democratic government, not a Tory one
Robert Sallis, Deborah Rohm Young, Sara Y Tartof, James F Sallis, Jeevan Sall, Qiaowu Li, Gary N Smith, Deborah A Cohen. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients. British Journal of Sports Medicine, 2021; bjsports-2021-104080 DOI: 10.1136/bjsports-2021-104080































What are the most common misconceptions about furniture free? Well these are my top three!