Why Wearing A Mask Isn’t Harmless
A compendium of mask-related information.
My intention is to help you make educated choices based on knowledge and not driven by emotion - don’t make your decisions based on the advice of those who won’t have to live with the results of those decisions. It’s far from exhaustive, but I’ve compiled it to help you inform yourself about the issues and give you a brief overview of the arguments for and against wearing them.
Please note that I wrote this in June 2020 and more and more studies are being censored and disappearing into the memory hole - if any links aren’t working then I apologise!
A Brief History Of Surgical Masks
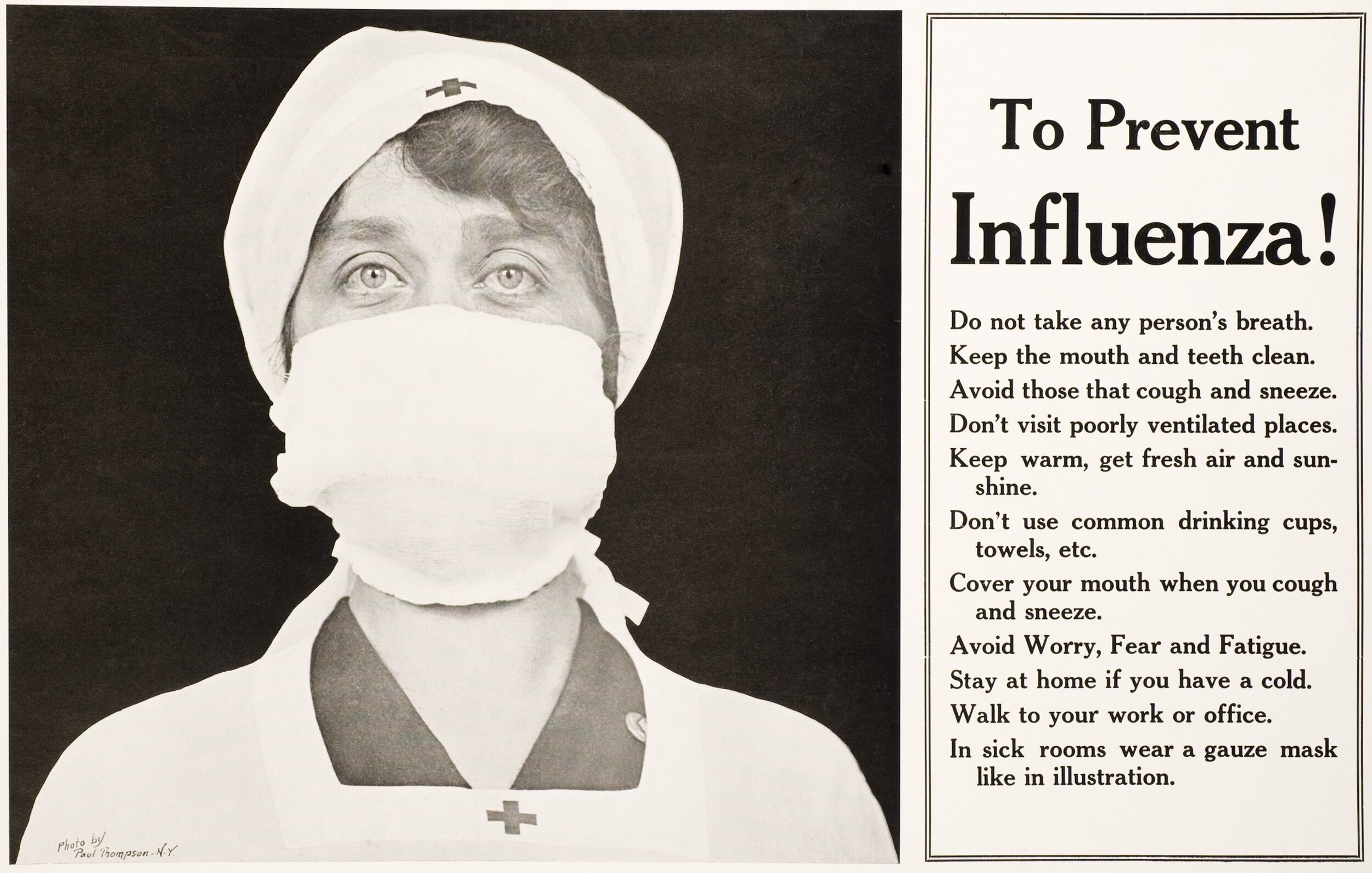
Wearing a surgical mask for infection control is thought to have begun in 1897 when Johann von Mikulicz-Radecki described a mask comprised of a layer of gauze. The same year Carl Flugge demonstrated that exhaled droplets could transmit tuberculosis and in 1898 Dr W. Hübener recommended that masks for surgery be made of two layers of gauze, worn at a distance from the nose, be used during operations. In 1905 Dr Alice Hamilton proposed that scarlet fever was transmitted through droplet infection and recommended that masks be worn by during surgery because of the danger of droplet infection from the mouth and nose and this was echoed by Lord Moynihan in 1906 who also advocated the use of masks during operations.
In 1915 Dr. Meltzer advised that masks of fine mesh gauze be used to cover the faces of patients with infantile paralysis and the faces of personnel attending them and, in 1918, George H. Weaver reported that over a two-year period the incidence of diphtheria contracted by attendants of infected patients was reduced to zero after wearing masks of double thickness gauze. He coupled this with a recommendation to sterilise the mask after each use and replace with a sterile one when it became moist and cautioned against hands being placed on the mask.
With the introduction of antibiotics in the 1940’s, and their rapid acceptance as a means of controlling infection, interest in surgical masks decreased. The rationale for wearing surgical face masks has shifted from protection of the patient to protection of the health professional.
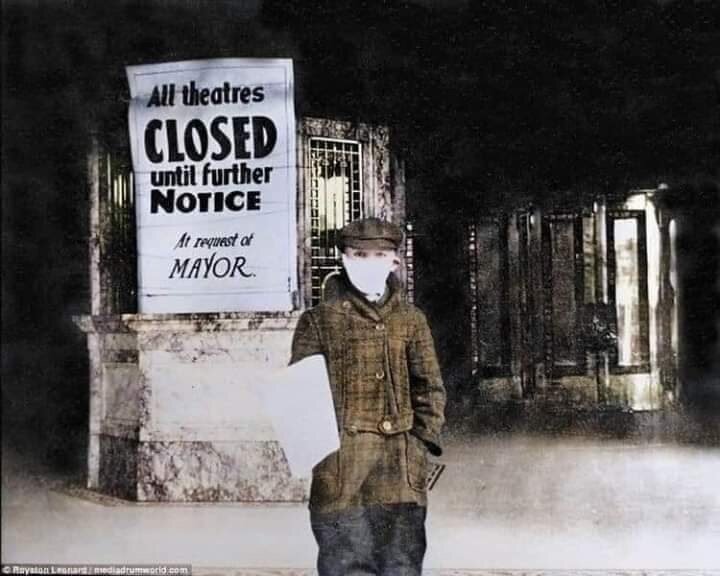
The 1918 Spanish Flu and The rise of the anti-Mask league
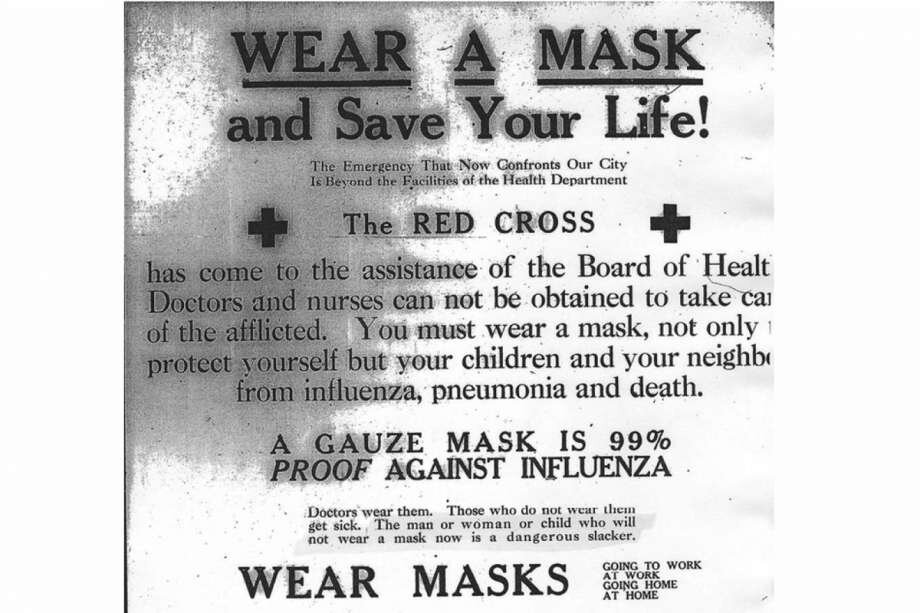
In America, the arrival of the Spanish Flu let to huge restrictions including the closure of department stores, barber shops, theatres, schools and churches as well as regulations on social distancing. Mirroring the mainstream hysterical reporting of today, The Red Cross placed advertisements in newspapers urging people to:
“WEAR A MASK and Save Your Life!
Doctors wear them, Those who do not wear them will get sick.
The man or woman or child who will not wear a mask is now is a dangerous slacker.”
In San Francisco a resolution was passed on October 25th 1918 which made mask wearing mandatory with the threat of fines and imprisonment. This lasted about a month until November 21st, 1918; however, when cases of the flu began increasing, a new ordinance mandating masks took effect on January 17th, 1919 and this galvanised the public to act. The Anti-Mask League was formed and by January 25th 1919, 5,000 people gathered at a roller skating rink for a public event hosted by the league designed to put an end to the law mandating that residents wear masks in public. The league submitted a petition to the city calling for the mask ordinance to end and on February 1st, on the recommendation of the Board of Health, San Francisco lifted the mask requirement.
In Tucson, Arizona, a banker insisted on going to jail instead of paying his fine for not masking up. In other western states, judges regularly refused to wear them in courtrooms. In New South Wales, reports of violations flooded newspapers immediately after masks were made compulsory. People were fined for sneezing, coughing, kissing and even talking outdoors and influenza police rounded up children playing outside and, in one day, 100 people in San Francisco were arrested for disobeying the mask order. A local newspaper helpfully noted that:
“When the maskless ones found that the police meant business all manner of excuse were advanced for not wearing masks, the favorite excuse being that the mask had just been removed to permit of smoking.”
This differed from the UK approach, where masks were advised as a precautionary measure for certain groups in large cities. Questions within the scientific community about the efficacy of mask wearing began around March 1919, with most UK scientists against them and The Lancet calling masks a ‘dubious remedy.’
Covid-19 | Mixed Messaging Since The Beginning
October 2014: In an interview with NBC News, Dr. Fauci urged state officials to avoid mandatory quarantines for healthcare workers returning to the U.S. after helping with the Ebola crisis in West Africa. ‘You don’t have to put them in a confined place,’ he says, after stating that socially isolating people who aren’t sick could lead to ‘unintended consequences.’
Note: Ebola has a fatality rate of around 50% compared to 0.8% for Covid-19.
March 8th: In an interview with Dr. Anthony Fauci (director of the National Institute of Allergy and Infectious Diseases) told 60 Minutes “There's no reason to be walking around with a mask.”
March 19th: Covid-19 is no longer considered to be a high consequence infectious disease (HCID) in the UK.
March 24th: The WHO released this video which tentatively recommended the wearing of masks, in combination with other protective measures.
April 3rd: The CDC announces the use of non-medical face coverings for the general public.
April 4th: The WHO updated this video with the caption that masks should only be worn by persons exhibiting symptoms of COVID-19.
April 6th: The WHO updated its advice. Now, apparently, there was no point in wearing masks:
“There is currently no evidence that wearing a mask by healthy persons in the wider community setting, including universal community masking, can prevent them from infection with respiratory viruses, including Covid-19.”
April 19th: BBC Radio Two presenter Jeremy Vine posted to his 739,000 followers on Twitter explaining why you should not wear a mask to protect yourself against the coronavirus. “1. You touch your face more. You may even touch under the mask because your nose and lips itch. 2. Masks become dirty, and could well be a place where germs gather, like the handkerchief you’ve kept in your pocket every day this week.” His third reason was that masks are needed by doctors and nurses and that any mask worn by a non-medical person is a mask ‘stolen’ from the NHS: “If 45 million members of the public decide they need masks, what does the health service do?”.
May 22nd: Good Morning Britain health expert Dr Hilary warned against wearing a protective mask while out running. “There’s no guidance to suggest your should wear a mask or it’s beneficial. In fact, it’s covering your mouth and your nose, it’s inhibiting your breathing to some extent and some people would say you’re rising the rate of levels of carbon dioxide you’re breathing out when you’re exercising and that’s probably not a good idea.”
May 27th: Dr. Anthony Fauci revealed he wears a mask “because I want to make it be a symbol for people to see that that’s the kind of thing you should be doing.” He told CNN, “I wear it for the reason that I believe it is effective, it’s not 100% effective. I mean, it’s sort of respect for another person, and have that other person respect you.”
June 5th: In its latest official guidance the WHO has recommended that everyone should wear masks in public areas. The WHO’s technical lead expert on Covid-19, Maria Van Kerkhove, said in a Reuters interview: “We are advising governments to encourage that the general public wear a mask." This was also contradicted the same day with the release of another WHO publication entitled Advice On The Use Of Masks In The Context Of Covid-19 : ‘There is limited evidence that wearing a medical mask by healthy individuals in households, in particular those who share a house with a sick person, or among attendees of mass gatherings may be beneficial as a measure preventing transmission.’
June 5th: Dr. Anthony Fauci said he has ‘no doubt’ that Americans who aren’t wearing face masks are increasing the risk of spreading the Covid-19.
June 15th: Mask wearing is mandatory for people travelling on public transport in the UK and operators will be able to refuse travel or issue penalty fines for
June 15th: Mask wearing is mandatory for people travelling on public transport in the UK and operators will be able to refuse travel or issue penalty fines for those who fail to wear a face covering.
June 16th: The WHO update their Mythbusters page which includes the following: ‘FACT: People should NOT wear masks when exercising, as masks may reduce the ability to breathe comfortably. Sweat can make the mask become wet more quickly which makes it difficult to breathe and promotes the growth of microorganisms. The important preventive measure during exercise is to maintain physical distance of at least one meter from others.’
July 12th: UK Cabinet Minister Michael Gove said he did not believe that face masks should be made a requirement in shops. “I don’t think mandatory, no, I think that it is basic good manners, courtesy and consideration, to wear a face mask if you are, for example, in a shop.” He added: “I trust people’s good sense.”
July 24th: Mask wearing is mandatory for people in the UK when they go shopping with penalty fines of up to £100 for non-compliance.
August 3rd: In Victoria, Australia, they announce they are in a State of Disaster and enter Stage 4 Lockdown. This is one of the strictest in the world and the maximum fine for breaching any of the many orders currently stands at $4,999.
August 6th: Los Angeles Mayor Eric Garcetti authorised the city to shut off water and power to home and businesses that are hosting large, unauthorised gatherings.
August 7th: The CDC updates its information about masks, saying that masks with exhalation valves or vents should not be worn to help prevent the person wearing the mask from spreading Covid-19 to others. This is because ‘masks with one-way valves or vents allow air to be exhaled through a hole in the material, which can result in expelled respiratory droplets that can reach others. This type of mask does not prevent the person wearing the mask from transmitting COVID-19 to others. Therefore, CDC does not recommend using masks for source control if they have an exhalation valve or vent.’ The CDC also says ‘there is currently not enough evidence to support the effectiveness of face shields for source control. Therefore, CDC does not currently recommend use of face shields as a substitute for masks.’
August 12th: The Department of Health and Social Care (DHSC) in the UK reduces the Covid-19 death toll by 10% - which accounts for more than 5,000 people - following a review of how figures are calculated.
August 14th: The UK Government removes 1.3 million Covid-19 tests from official England figures due to alleged ‘double counting’.
August 14th: The UK Government increases the fines to £3,200 for people who ‘repeatedly refuse to wear a face mask.’
August 28th: In Holland, Amsterdam and Rotterdam have dropped a pilot scheme requiring face coverings in the busiest areas. Since the mask trial began, the main shopping streets in these two cities have seen visitor numbers fall by almost a third, according to a survey. Instead they are asking people to maintain social distancing of 1.5m (5ft).
October 13th: Doctors in France are refusing to treat women who are in labor unless they wear a mask throughout. This has caused vomiting, hyper-ventilation and some women have said the stress has led to them requiring a caesarean.
Nov 15th: Anthony Fauci told CNN’s State of the Union that social distancing and masks will still be necessary even if you take a vaccine: “Obviously, with a 90+% effective vaccine, you could feel much more confident, but I would recommend to people to not abandon all public health measures just because you’ve been vaccinated.”
December 8th: The first face mask discrimination case in the UK has led to compensation of £7,000 by a service provider who refused her access to a service because she was unable to wear a face mask. The pay-out was achieved through negotiation as there was no dispute that access had been denied, or that the Claimant had a disability exemption. The only thing to be agreed was the amount of compensation, not whether it was due or not.
January 5th: Judicial Watch announced that it received 848 pages of documents revealing the contract materials and communications related to a $1 billion contract for face masks between the California Office of Emergency Services and the Chinese Communist Party linked BYD. The documents reveal that the Office of Emergency Services Assistant Chief Counsel admits that they deviated from their normal procurement process for this contract. Additionally, in the contract between Office of Emergency Services and BYD, BYD uses a different name, Global Healthcare Product Solutions, LLC., and BYD provides no liability or warranty for the masks if they are faulty.
Jan 12th: Tesco, Sainsbury’s and Morrisons have said they will no longer grant entry to shoppers without a face covering. It comes amid fears supermarkets could become hotspots for spreading Covid-19.
Jan 13th: SAGE released a document, which it endorsed, saying that masks were primarily a source control (cloth and surgical masks are thought to offer the wearer little protection) and citing an estimate for their typical impact on transmission of 6-15%.
Jan 25th: Dr Fauci is now saying that double-masking makes ‘common sense’ and is likely more effective. The New York Times states that two masks are the new masks and ‘is a sensible and easy way to lower your risk when you have to spend more time around others’. They show you how to wear them here.
Jan 27th: A report on CNBC talks about the effectiveness of triple-masking.
Feb 23rd: 70 doctors in Belgium call masks a ‘major threat’ to children’s development. 100 UK health professionals- psychologists, academics and paediatricians- say that masks for children are ‘not only unnecessary but potentially harmful’.
March 2nd: Oxford professor Trish Greenhalgh has said joggers should be wearing facemasks while out running.“There is no doubt the virus is in the air, there is no doubt that you can catch it if you inhale, air that someone else has exhaled...The exercising jogger - the puffing and panting jogger - you can feel their breath come and you can sometimes actually feel yourself inhale it, so there’s no doubt that there is a danger there...So you’re jogging along, you think you’re fine, and then the next day you develop symptoms of Covid, but you’ve actually breathed that Covid onto someone perhaps an old lady walking a dog or something like that.”
March 2nd: A London council has become the first to tell all primary schools in its area that children should wear face masks all day. Redbridge Council in east London has written to all 56 primaries under its control, advising that masks should be worn by pupils as young as four all day apart from when they are eating.
March 21st: People may need to wear face coverings and socially distance for several years until we return to normality, Mary Ramsay, the head of immunisation at Public Health England stated, claiming it was needed to ‘allow the economy to function’.
March 25th: Masks and social distancing could be in place for 10 years as ‘it’s politically unrealistic to expect the Government to backtrack now’ former Supreme Court judge Lord Sumption warns.
April 1st: The Spanish government has passed a controversial law which makes face masks mandatory in all outdoor settings, including beaches, swimming and in nature and they must be worn at all times. The measure has no end date, but will last until the Government declares the Covid-19 crisis over, the announcement added. Without clear details on how the policy will be enforced, tourists could open themselves up to fines by swimming in the sea without a face covering.
(Perhaps it’s an April fools? We can only hope so)
May 10th: Dr Fauci says he hopes America will be ‘as close to back to normal as we can’ by Mother's Day 2022 and Americans may start wearing masks seasonally, claiming that: ‘We’ve had practically a non-existent flu season this year merely because people were doing the kinds of public health things that were directed predominately against Covid-19. So it is conceivable that as we go on, a year or two or more from now, that during certain seasonal periods when you have respiratory-borne viruses like the flu, people might actually elect to wear masks to diminish the likelihood that you’ll spread these respiratory-borne diseases.’
May 11th: Dr Fauci appears on Good Morning America and admits that his post-vaccination mask-wearing was meant to serve as a ‘signal’ - rather than a genuine attempt to stem the spread of Covid-19.
May 13th: The CDC issues new guidance saying that if you identify as being ‘fully vaccinated’ you do not need to wear masks in most indoor places.
June 4th: A FOIA request resulted in the release of nearly 3,000 emails sent by Dr Fauci from early February 2020 through May 2020. Read what Fauci was saying privately about masks, therapeutics, vaccines, ventilators, and many other COVID-19 topics here.
July 17th: Dr Colin Axon, a scientific adviser to SAGE, accused medics of presenting a “cartoonish” view of how tiny particles travel through the air “Medics have this cartoonised view of how particles move through the air – it’s not their fault, it’s not their domain – they’ve got a cartoonish view of how the world is,” he said. “The public were demanding something must be done, they got masks, it is just a comfort blanket,” Dr Axon noted. “But now it is entrenched, and we are entrenching bad behaviour.”
July 27th: The CDC now recommends that fully vaccinated people return to wearing masks indoors in parts of the U.S. where the coronavirus is surging.
1st August: Dr Fauci now says that people who don’t wear masks are ‘encroaching on others’ individual rights’ as he defends the new CDC mask guidance.
Evidence for the use of masks
2021: This study looked at the positive effects of mask-wearing and also concluded that, “in addition to protecting the health of their patients, doctors should also base their actions on the guiding principle of the 1948 Geneva Declaration, as revised in 2017. According to this, every doctor vows to put the health and dignity of his patient first and, even under threat, not to use his medical knowledge to violate human rights and civil liberties. Within the framework of these findings, we, therefore, propagate an explicitly medically judicious, legally compliant action in consideration of scientific factual reality against a predominantly assumption-led claim to a general effectiveness of masks, always taking into account possible unwanted individual effects for the patient and mask wearer concerned, entirely in accordance with the principles of evidence-based medicine and the ethical guidelines of a physician.”
2020: This meta-analysis notes that:
“Our findings continued to support the ideas not only that masks in general are associated with a large reduction in risk of infection from SARS-CoV-2, SARS-CoV, and MERS-CoV but also that N95 or similar respirators might be associated with a larger degree of protection from viral infection than disposable medical masks or reusable multilayer (12–16-layer) cotton masks. Nevertheless, in view of the limitations of these data, we did not rate the certainty of effect as high. Our findings accord with those of a cluster randomised trial showing a potential benefit of continuous N95 respirator use over medical masks against seasonal viral infections.”
2020: A systematic review compared standard surgical masks and respirator masks, which included a single small trial from 2009 of respirator masks, standard masks, and no masks among the general public during an influenza epidemic in Australia. That trial showed a benefit of masks over no masks, but no benefit of respirator masks over standard ones, and also showed that masks were worn less than 50% of the time.
2020: This evidence-based review concluded:
‘Although no direct evidence indicates that cloth masks are effective in reducing transmission of SARS-CoV-2, the evidence that they reduce contamination of air and surfaces is convincing.’
2011: This review covered physical interventions and included 67 studies:
“We found limited evidence of the superior effectiveness of devices such as the N95 respirator over simple surgical masks. This evidence is supported by a high quality hospital‐based trial which reports non‐inferiority between face barriers. Overall masks were the best performing intervention across populations, settings and threats. More expensive and uncomfortable (especially if worn for long periods) than simple surgical masks, N95 respirators may be useful in very high‐risk situations but additional studies are required to define these situations.”
2010: A 2010 systematic review of face masks in influenza epidemics, which included respirator masks and standard surgical masks. It found some efficacy of masks if worn by those with respiratory symptoms but not if worn by asymptomatic individuals.
2007: A systematic review and expert panel deliberation acknowledged the difficulties in interpreting evidence and stated:
“With the exception of some evidence from SARS, we did not find any published data that directly support the use of masks … by the public.”
According Dr. Brosseau (a national expert on respiratory protection and infectious diseases) and Dr. Sietsema (an expert on respiratory protection) some of these studies fail to recognise several important facts:
The filter performance of a cloth material does not directly translate or represent its performance on an individual, because it neglects the understanding of fit.
Cloth masks or coverings come in a variety of shapes, sizes, and materials and are not made according to any standards.
Transmission is not simply a function of short random interactions between individuals, but rather a function of particle concentration in the air and the time exposed to that concentration.
Evidence Against
2021: In this cohort study, patients were recruited as part of a randomised controlled trial. ‘We did not find any evidence of decreased risk of transmission in individuals who reported mask use. We assessed risk of transmission and developing symptomatic disease and incubation dynamics using regression analysis. We assessed the relationship of viral load and characteristics of cases (age, sex, number of days from reported symptom onset, and presence or absence of fever, cough, dyspnoea, rhinitis, and anosmia) and associations between risk of transmission and characteristics of the index case and contacts.’
2021: In this study, the blue, cloth surgical masks were found be only 10% effective in preventing a Covid-19 infection. With familiar cognitive dissonance, the study leader said, ‘There is no question it is beneficial to wear any face covering, both for protection in close proximity and at a distance in a room,’ followed by a reminder, ‘however, there is a very serious difference in the effectiveness of different masks when it comes to controlling aerosols.’
2021: A new randomised clinical trial published in the Journal of the American Medical Association found that the air masked children inhaled contained more than six times the legal safe limit for closed rooms as set down by the German Federal Environmental Office. The safe limit is 0.2%, whereas the air the masked children inhaled contained over 1.3% carbon dioxide. The effect was worse for younger children, with one seven year-old child inhaling air with 2.5% carbon dioxide, over 12 times the safe limit. The study looked at two types of mask, FFP2 masks and surgical masks, and found no significant difference between the two.
2021: D. G. Rancourt publishes a working technical report of the ‘Review of scientific reports of harms caused by face masks, up to February 2021’.
2020: A review of the literature that was published in the CDC journal Emerging Infectious Diseases did not find evidence that masks were protective against influenza. Masks did not help infected people reduce their risk of infecting others, nor reduce the risk of uninfected people contracting influenza:
‘In this review, we did not find evidence to support a protective effect of personal protective measures or environmental measures in reducing influenza transmission..We did not find evidence that surgical-type face masks are effective in reducing laboratory-confirmed influenza transmission, either when worn by infected persons (source control) or by persons in the general community to reduce their susceptibility’.
They also admitted that ‘the mechanisms of person-to-person transmission in the community have not been fully determined. Controversy remains over the role of transmission through fine-particle aerosols. Transmission by indirect contact requires transfer of viable virus from respiratory mucosa onto hands and other surfaces, survival on those surfaces, and successful inoculation into the respiratory mucosa of another person. All of these components of the transmission route have not been studied extensively.’
2020: The first randomised control trial of the real-world efficacy of face masks against Covid-19 infection took place in Denmark with 6,000 participants. The study used ‘high-quality surgical masks with a filtration rate of 98%’ and the trial found no statistically significant benefit of wearing a face mask. It found a 2.1% vs 1.8% infection rate for unmasked vs masked groups (with around 3,000 participants in each group initially). However, due to low virus prevalence these figures correspond to only 53 and 42 participants respectively so the authors had to state that the result is not statistically significant (too few infections to be confident it’s not random).
2020: Two studies (here and here) suggests that in some cases the virus can enter the brain, potentially via the olfactory nerves and connect directly with the area of the brain dealing with recent memory and memory consolidation. Through wearing a mask, the exhaled viruses will not be able to escape and will concentrate in the nasal passages, which may lead to them being able to enter the olfactory nerves and travel into the brain.
2020: This review paper concluded by saying that “Wearing face masks may reduce primary respiratory infection risk, probably by 6-15%. It is important to balance evidence from RCTs and observational studies when their conclusions widely differ and both are at risk of significant bias. Covid-19-specific studies are required.” They also say “The environmental and economic costs of regularly using face masks are notable, and only partly abated by reuse.”
2020: This study looked whether there was shedding of fibres from disposable and reusable masks. Research on synthetic fibres has shown a correlation between the inhalation of synthetic fibres and various bronchopulmonary diseases, such as asthma, alveolitis, chronic bronchitis, bronchiectasis, fibrosis, COPD, spontaneous pneumothorax and chronic pneumonia. They posit that it may also cause Pulmonary fibrosis which they claim ‘is among the worst diseases that can be suffered or witnessed. It kills exceedingly slowly, by ever-thickening matrix formation, a kind of scar tissue, obstructing the alveoli and reducing their air exchange. The illness worsens slowly over time, and suffocates the victim very gradually. Nothing is available to the sufferer from conventional medicine. Neither medication nor radiation can undo the damage of the fibrous matrix laid down in the lungs’ tissue. Similarly, surgery is not available to eliminate the insidious, suffocating mesh that painstakingly takes the life of the unfortunate patient. Neither is any known cure available in the realm of natural or alternative medicine. Neither nutrient, herb, nor any other known treatment can even reduce the fibrogenesis, let alone eliminate it. The 5-year survival rate is only 20%. The only remedy against this scourge is diligent prevention of small and microscopic inhaled foreign bodies.’
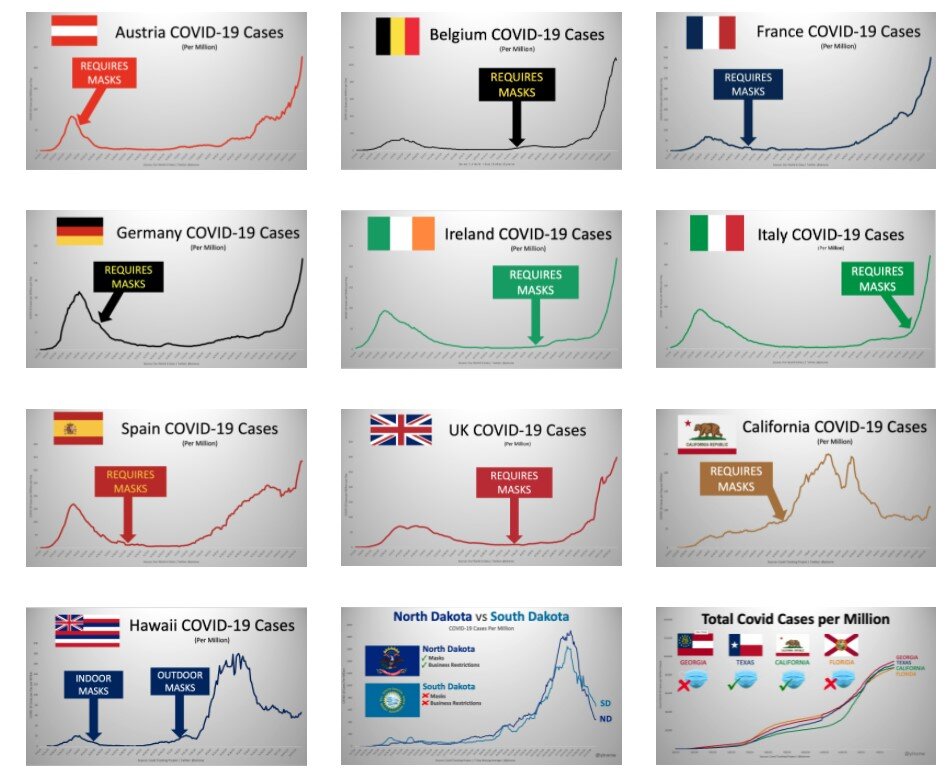
2020: This working paper focused on 25 U.S. states and 23 countries with more than 1,000 Covid-19 deaths (as of late July). They concluded that the data trends observed likely indicate that non-pharmaceutical interventions (NPIs) – such as lockdowns, closures, travel restrictions, stay-home orders, event bans, quarantines, curfews, and mask mandates – do not seem to affect virus transmission rates overall.
2020: This small scale study analysed 14 masks and coverings by using a tool that allowed researchers to track individual particles released from a person's mouth when they spoke the phrase “Stay healthy, people.” Speakers said the same phrase while wearing the different models of masks, and no masks at all, to compare. Each face covering was tested 10 times.
“The neck gaiter that we tested did essentially nothing, and worse than nothing, because it appeared to make large droplets into small droplets,” Isaac Henrion, the study's co-author, told CBS News. The experiment involved only a small number of speakers and face coverings, and the researchers stressed that more testing is needed - some gaiters might work better than others, depending on how they're made.
2020: The New England Journal of Medicine editorial on the topic of mask use versus Covid-19 assesses the matter as follows:
‘We know that wearing a mask outside health care facilities offers little, if any, protection from infection. Public health authorities define a significant exposure to Covid-19 as face-to-face contact within 6 feet with a patient with symptomatic Covid-19 that is sustained for at least a few minutes (and some say more than 10 minutes or even 20 minutes). The chance of catching Covid-19 from a passing interaction in a public space is therefore minimal. In many cases, the desire for widespread masking is a reflexive reaction to anxiety over the pandemic.’
2020: This study found that 624 out of 714 people wearing N95 masks left visible gaps when putting on their own masks. Of participants given N95 respirators with an instruction sheet and then asked to put one on, only about 13% passed the visual mask fit test.
2020: This review found that masks had no effect specifically against Covid-19, although facemask use seemed linked to, in 3 of 31 studies, ‘very slightly reduced’ odds of developing influenza-like illness.
2020: Plastic face shields are almost totally ineffective at trapping respiratory aerosols, according to modelling in Japan. A simulation using Fugaku, the world’s fastest supercomputer, found that almost 100% of airborne droplets of less than 5 micrometres in size escaped through plastic visors of the kind often used by people working in service industries.
2020: This CDC study, which surveyed symptomatic Covid-19 patients, has found that 70.6% of respondents reported ‘always’ wearing a mask, while an additional 14.4% say they ‘often’ wear a mask. That means 85% of infected Covid-19 patients reported habitual mask wearing. Only 3.9% of those infected said they ‘never’ wear a face covering.
2020: These researchers developed a computational face mask model using a physiologically realistic model of a person wearing a surgical mask with pleats and then using numerical methods to track the particles through the mask. They found that wearing a mask with low (less than 30%) filtration efficiency can be worse than not wearing a mask at all. “It is natural to think that wearing a mask, no matter new or old, should always be better than nothing. Our results show that this belief is only true for particles larger than 5 micrometers, but not for fine particles smaller than 2.5 micrometers,” said author Jinxiang Xi.
2020: The conclusion of this study notes that: ‘Medical face masks have a marked negative impact on cardiopulmonary capacity that significantly impairs strenuous physical and occupational activities. In addition, medical masks significantly impair the quality of life of their wearer. These effects have to be considered versus the potential protective effects of face masks on viral transmissions.’
2019: This randomised clinical trial of 2862 participants showed that both N95 respirators and surgical masks ‘resulted in no significant difference in the incidence of laboratory confirmed influenza.’
2018: This study shows a potential causation link between hypoxia and blood clotting and discovered that hypoxia down regulates expression of the important natural anticoagulant protein S. The level of protein S was found to drop by 50% when O2 levels were at 15%.
An N95 mask simulates a similarly low oxygen saturation, which could indicate that wearing a mask may decrease your natural ability to prevent blood clots by 50%.
2018: This study provides strong evidence for the identification that surgical masks are as source of bacterial contamination during operative procedures. It recommends surgeons should change their mask after each operation, especially those beyond 2 hours.
2018: This study looked at whether wearing a mask affected the Six Minutes Walking Test (6MWT) which is regularly used in pulmonology. They found that surgical mask wearers had significantly increased dyspnea (difficult or laboured breathing) after a 6-minute walk than non-mask wearers.
2016: A review of current research written from the perspective of the dental professional notes:
‘The primary reason for mandating the wearing of face masks is to protect dental personnel from airborne pathogens. This review has established that face masks are incapable of providing such a level of protection. Unless the CDC, national and provincial dental associations and regulatory agencies publically admit this fact, they will be guilty of perpetuating a myth which will be a disservice to the dental profession and its patients.’
2016: An article in The Journal of Biological Engineering notes that: ‘Wearing respirators come[s] with a host of physiological and psychological burdens. These can interfere with task performances and reduce work efficiency. These burdens can even be severe enough to cause life-threatening conditions if not ameliorated.’
2016: This meta-analysis found that both randomised controlled trials and observational studies of N95 respirators and surgical masks used by healthcare workers did not show benefit against transmission of acute respiratory infections. It was also found that acute respiratory infection transmission ‘may have occurred via contamination of provided respiratory protective equipment during storage and reuse of masks and respirators throughout the workday.’
2015: This study claimed to be the first randomised control trial of cloth masks and ‘the results caution against the use of cloth masks. This is an important finding to inform occupational health and safety. Moisture retention, reuse of cloth masks and poor filtration may result in increased risk of infection. Further research is needed to inform the widespread use of cloth masks globally.’
2015: A study in the British Medical Journal found that healthcare workers caught viruses from their patients 13 times more often if they wore a cloth mask than if they wore a medical mask.
2015: In this paper the authors look at whether there is evidence for the use of face masks during surgery and stated that ‘statistical analysis of the extracted data revealed no statistically significant association between mask usage and the incidence of surgical site infection. The study concluded that ‘it is unclear whether the wearing of surgical facemasks by members of the surgical team has any impact on surgical wound infection rates for patients undergoing clean surgery’.’
2012: This cross-sectional study was titled ‘Effect of face veil on ventilatory function among Saudi adult females’. It compared ventilatory function between niqab wearing and non-niqab wearing healthy Saudi females. The researchers speculated that the niqab wearing women may have adapted to shallow breathing patterns with a higher heart rate and that regular use may be one of the reasons of a high prevalence of fibromyalgia and cervicobrachialgia among Saudi females.
2012: This review of 17 studies found that:
‘None of the studies established a conclusive relationship between mask ⁄ respirator use and protection against influenza infection.’
2011: A study found that a medical mask was no more protective against viruses than wearing no mask at all.
2011: Experiments have shown that influenza or other coronaviruses can enter the eyes and travel to the nose and into the respiratory system - so face masks alone do not offer much protection unless combined with eye protection. Masks combined with goggles appear to provide complete protection in laboratory experiments yet there are no studies in real-world situations measuring the results of combined mask and eyewear.
2010: The N95 respirator was tested in use and the “dead-space oxygen and carbon dioxide levels did not meet the Occupational Safety and Health Administration’s ambient workplace guidelines.”
2009: According to doctors at the Harvard School of Public Health, the N95 respirator, recommended for medical workers, requires training to use properly and ‘without training, the masks could not only expose workers to the virus but also lull them into thinking they are protected.’
2009: A randomised controlled trial looked at the use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan and found that face mask use found to be not protective against the common cold, compared to controls without face masks among healthcare workers.
2003: Australian health authorities have warned that surgical masks may not be an effective protection against the SARS virus.
“Those masks are only effective so long as they are dry,” said Professor Yvonne Cossart of the Department of Infectious Diseases at the University of Sydney. “As soon as they become saturated with the moisture in your breath they stop doing their job and pass on the droplets.” Professor Cossart said that could take as little as 15 or 20 minutes, after which the mask would need to be changed. But those warnings haven’t stopped people snapping up the masks, with retailers reporting they are having trouble keeping up with demand. “I think they’re of marginal benefit, in a way they give some comfort to people who think they’re doing as much as they can do to prevent the infection.”
Adverse consequences of wearing masks
2020: This was a meta-analysis drawing from 72 years of literature. Curiously, this study is found on the CDC’s own website, directly contradicts recent advice from the CDC about wearing a mask:
“In our systematic review, we identified 10 RCTs that reported estimates of the effectiveness of face masks in reducing laboratory-confirmed influenza virus infections in the community from literature published during 1946–July 27, 2018….In pooled analysis, we found no significant reduction in influenza transmission with the use of face masks…Our systematic review found no significant effect of face masks on transmission of laboratory-confirmed influenza….Proper use of face masks is essential because improper use might increase the risk for transmission.”
2020: The rise of ‘mask mouth’. Dentists are seeing patients coming in with issues related to prolonged use of mask wearing. “Gum disease - or periodontal disease - will eventually lead to strokes and an increased risk of heart attacks,” Marc Sclafani, a dentist and co-founder of One Manhattan Dental, told the New York Post. Increases in inflammation and cavities are thought to be connected to mouth breathing when wearing a mask which causes a dry mouth, a decrease in saliva and contributes to a buildup of bad bacteria.
2020: A German University has set up an online registry and this study is based on the data of 25,930 children. The average wearing time of a face mask was 270 minutes per day per child. Impairments caused by wearing the mask were reported by 68% of the parents. These included irritability (60%), headache (53%), difficulty concentrating (50%), less happiness (49%), reluctance to go to school/kindergarten (44%), malaise (42%) impaired learning (38%) and drowsiness or fatigue (37%). It ends by saying that ‘adults need to collectively reflect the circumstances under which they would be willing to take a residual risk upon themselves in favour of enabling children to have a higher quality of life without having to wear a mask.’
2020: A study from Singapore found an increased risk of headaches among healthcare workers:
“Of the 158 respondents, 81% reported headaches when they wore either the N95 face mask, with or without the protective eyewear. All respondents described the headaches as bilateral in location….Interestingly, the location of the discomfort experienced by the participants corresponded to the areas of contact from the face mask or goggles and their corresponding head straps. The majority 87% reported a sensation of pressure or heaviness at the affected sites, with some 11% characterizing it as a throbbing or pulling pain…Since COVID-19 outbreak, 91% of respondents with pre-existing headache diagnosis either “agreed” or “strongly agreed” that the increased PPE usage had affected the control of their background headaches, which affected their level of work performance.”
2020: Lloyds Pharmacy has produced a guide for dealing with ‘Maskne’, skin breakouts caused by the rubbing of masks against the skin leading to micro-tears. These enable bacteria, dirt and oil to enter the skin. Lack of air circulation encourages bacteria growth and can lead to blackheads, whiteheads or pimples that will vary in size depending on how infected they become.
2020: An article posted in Ophthalmology and Therapy highlights eye dryness, irritation and keratopathy (a corneal disease) as a result of prolonged mask-wearing, dubbed ‘Mask eye’. Mask-associated ocular irritation raises concerns about eye health and increased risk of disease transmission in prolonged mask users.
2020: According to a new study, influenza infections can lead to an increased risk of bacterial pneumonia. Influenza is caused by a virus, but the most common cause of death is secondary bacterial pneumonia rather than the influenza virus per se. Pneumococcal infections are the most common cause of community-acquired pneumonia and a leading global cause of death.
2020: According to the CDC's Morbidity and Mortality Weekly Report, a New Jersey hospital saw increase of hospital-acquired bacterial infection between February and July.
2020: Dr. Meehan speculates that the increase in bacterial pneumonias being reported at Emergency Rooms and urgent care centres could be connected to face mask wearing.
2015: A study in the BMJ showed that people who were told to wear cloth masks for extended periods of time (for the purposes of the study) had higher rates of influenza-like illness (“ILI”) than other healthcare workers who could decide if and when to wear masks, and had higher rates of ILI than those wearing surgical masks:
“The rates of all infection outcomes were highest in the cloth mask arm, with the rate of ILI statistically significantly higher in the cloth mask arm [13 times higher] compared with the medical mask arm. Cloth masks also had significantly higher rates of ILI compared with the control arm [workers who followed standard practice, which could sometimes include mask wearing]. An analysis by mask use showed ILI and laboratory-confirmed virus were significantly higher [6.64 times for ILI and 1.72 times higher for lab confirmed virus] in the cloth masks group compared with the medical masks group. Penetration of cloth masks by particles was almost 97% and medical masks 44%.”
2009: This study noted that:
“N95-masked health-care workers were significantly more likely to experience headaches. Face mask use in health-care workers was not demonstrated to provide benefit in terms of cold symptoms or getting colds.”
Masks are useless if worn incorrectly
Since the SARS epidemic in 2003, Asia has developed has a strong culture of wearing masks, both in public and medical settings. They are worn as a courtesy to stop spreading infections if people are sick; protecting others is seen as a civic duty. Europe doesn’t have the same culture of mask-wearing which is probably why, when you go out and about, you see many people wearing masks incorrectly - fiddling, pulling them down to talk, have it underneath their nose or hang it up in their car whilst they go about their day.
Below are the UK Government guidelines of how to wear a mask correctly:
Wash your hands or use hand sanitiser before putting it on and after taking it off.
Avoid touching your eyes, nose, or mouth at all times and store used face coverings in a plastic bag until you have an opportunity to wash them.
Do not touch the front of the face covering, or the part of the face covering that has been in contact with your mouth and nose.
Once removed, make sure you clean any surfaces the face covering has touched.
You should wash a face covering regularly. It can go in with other laundry, using your normal detergent.
- How to wear and make a cloth face covering, Public Health England
The Health and Safety Executive (HSE) recommend wearing respiratory protective equipment (RPE) for less than an hour before taking a break and, if it needs to be worn continuously, to use tight-fitting powered or constant-flow airline breathing apparatus. It is also a legal requirement that workers wearing (RPE) should be face fit tested to the HSE standard.
The Environmental cost of masks
Polypropylene is listed as the ingredient that some of the surgical disposable masks are made of. There is a chance these masks may contain volatile organic compounds (VOCs) which, when inhaled, cause headache, allergies, dizziness, or nausea. Polypropylene is chemically synthesised from ethylene, a compound that's made from petroleum or natural gas and it is estimated that it takes about 20-30 years to degrade in landfill and, it can be considered to be biodegradable, although this doesn’t mean they are safe for the environment since all plastics contain harmful toxins that will leach into the soil when broken down.
There has been much talk of mask-wearing and little talk of mask-disposing. The Plastic Waste Innovation Hub reports that the UK is expecting an extra 66,000 tonnes of contaminated waste from face coverings alone in 2020. Masks accumulate significant quantities of viral particles and couple this with a study which showed that Covid-19 can survive up to 7 days on the surface of face masks surely means that masks should be considered as clinical waste. Presumably the Government is gearing up to set up suitable clinical waste disposal points to allow safe disposal of them?
An NGO called Opération Mer Propre (Operation clean sea) works in cleaning underwater waste from the Mediterranean sea around the Antibes region in southern France and has spoken out about the new Covid-19 pollution, which adds to the already chronic problem of plastic pollution; “these masks, we haven't had them for long, and we're going to have billions, so I say watch out, it's the beginnings of a new type of pollution…this is only the beginning and if nothing changes it will become a real ecological disaster and maybe even sanitary one.”
The Asian Development Bank estimates that during the peak of the Covid-19 outbreak, Manila could have been generating up to 280 tonnes of extra medical waste per day much of which washed up washed up on coral reefs close to the Philippine capital.
According to new research, a survey of 2,000 people found that over half (51%) were using single-use blue surgical face masks. Therefore, the UK could be sending as many as 54.5 million single-use face masks to landfill every single day and 1.6 billion every month. If the global population adheres to a standard of one disposable face mask per day after lockdowns end, the pandemic could result in a monthly global consumption and waste of 129 billion face masks and 65 billion gloves, 6 months adds up to 74 billion face masks being used and 12 months equates to an eye-watering 1 trillion 548 billion face masks disposed of worldwide.
The Toxic cost of Reprocessing masks
Medline Industries is America’s largest provider of medical supplies and in March they were using ethylene oxide to decontaminate and reprocess 100,000 masks a day. It is commonly used as a sterilizing agent in manufacturing plants that make medical products and at least half of U.S. medical devices are sterilised using this gas, which is regulated via the Food and Drug Administration. Ethylene oxide is is toxic and exposure to high levels may cause significant harm, particularly to aquatic organisms. It does not accumulate in the environment, but its breakdown in air and water is fairly slow.
The Environmental Protection Agency states that:
“Acute inhalation exposure of workers to high levels of ethylene oxide has resulted in nausea, vomiting, neurological disorders, bronchitis, pulmonary edema, and emphysema…Ethylene oxide is carcinogenic to humans and that exposure to ethylene oxide increases the risk of lymphoid and breast cancer.”
The CDC warns that ethylene oxide is carcinogenic and teratogenic, and that “inhalation of ethylene oxide has been linked to neurologic dysfunction and may cause other harmful effects to the wearer.” and admits that “the effectiveness of reprocessing methods to inactivate coronavirus (or other enveloped virus) on a medical mask and on preserving the integrity of the mask has not been established to date.”
The Occupational Safety and Health Administration states that:
“In addition to eye pain and a sore throat, exposure can cause difficult breathing and blurred vision. Exposure can also cause dizziness, nausea, headache, convulsions, blisters and can result in vomiting and coughing. Both human and animal studies show that ethylene oxide is a carcinogen that may cause leukemia and other cancers. Ethylene oxide is also linked to spontaneous abortion, genetic damage, nerve damage, peripheral paralysis, muscle weakness, as well as impaired thinking and memory.”
In April, the Washington State Nurses Association filed a complaint with Department of Occupational Safety and Health demanding an immediate halt to the reusing of any face masks that have been decontaminated by the ethylene oxide cleaning process.
Potentially toxic masks distributed in schools and daycares in Canada
The Canadian Broadcasting Corporation published the following article, which I’ve edited for brevity:
One model of mask distributed to Quebec schools and daycares may be dangerous for the lungs as they could contain a potentially toxic material. Health Canada warned of the potential for ‘early pulmonary toxicity’ from the SNN200642 masks which are made in China and sold and distributed by Métallifer, a Quebec-based manufacturer. They conducted a preliminary risk assessment which revealed a potential for early lung damage associated with inhalation of microscopic graphene particles. Graphene is a strong, very thin material that is used in fabrication, but it can be harmful to lungs when inhaled and can cause long-term health problems.
This is not the first time masks distributed to daycares have been recalled. Between May and November 2020, the health ministry distributed 31.1 million MC9501 masks throughout the network to protect staff from Covid-19, but they were determined to be unfit for use and in December 2020, the Quebec government revealed that masks it had been distributing for months to more than 15,000 daycares across the province did not meet safety standards, and daycare staff were ordered to stop using them.
Try it at home: the pulse oximeter test
A pulse oximeter measures how much light is absorbed by your blood and reveals how much oxygen your blood contains. It shines 2 lights through your fingertip or earlobe: one red light and one infrared light. The oximeter display shows the percentage of oxygen in your blood so for someone who’s healthy, the normal blood oxygen saturation level will be around 95–100%. If the oxygen level is below this, it can be an indicator that there is a lung problem.
i. Take an initial reading.
ii. Wear your mask for 15 minutes
iii. Take another reading and note if there is much difference or if you blood oxygen saturation level has dropped to less than 95%.
Abnormally low blood oxygen levels are known as hypoxia and is associated with an impairment in immunity. Studies have shown that hypoxia may inhibit the type of main immune cells used to fight viral infections, this puts you at an increased risk of contracting infections.
Timeline Of Mask Mandates And Restrictions Being Lifted
2020
28th September: Florida lifts Covid-19 restrictions on all businesses in the state, including restaurants and bars and no further fines for not wearing face masks will be issued.
2021
Jan 18th: North Dakota mask mandate is lifted. The North Dakota House of Representatives passed a bill that would make mandatory mask wearing illegal.
Feb 7th: Iowa mask mandate is lifted.
Feb 12: Montana mask mandate is lifted.
March 3rd: Mississippi mask mandate is lifted along with all Covid-19 restrictions and mask mandates, with businesses able to reopen at full capacity.
March 5th: South Carolina never had a statewide mask mandate, but ended mandatory requirements that they be worn in restaurants and State Government buildings.
March 5th: Arizona ends indoor capacity restrictions at state venues including restaurants, gyms, theatres, water parks, bowling alleys, and bars providing dine in services. The State never had a mask mandate because, as Gov. Steve Ducey said, ‘we always knew that fighting this virus would be dependent on the personal responsibility of everyday Arizonans.’
March 6th: West Virginia keeps the mask mandate but bars and restaurants are able to operate at full seating capacity, though some restrictions on standing room congregation remain in effect.
March 30th: Arkansas mask mandate is lifted.
March 19th: Connecticut lifts indoor capacity restrictions at dining establishments, libraries, museums, gyms, retail, offices, and houses of worship but doesn’t lift the mask mandate.
March 10th: Texas mask mandate is lifted along with all Covid-19 restrictions and mask mandates, with businesses able to reopen at full capacity.
March 11th: Texas Attorney General sues city of Austin for keeping its mask mandate.
March 11th: Oklahoma has been fully reopened since June 2020 with no mask mandate and this week the Governor issued a new executive order ending statewide restrictions on events and also allows for people to enter state buildings without needing to wear a mask.
‘We want to get our summer back. But also at the same time, we are telling Oklahomans to take personal responsibility, continue to be vigilant. And I think Oklahomans will do the right thing.’
March 16th: Wyoming mask mandate is lifted.
April 6th: Indiana mask mandate is lifted.
April 9th: Alabama mask mandate is lifted.
April 10th: Utah’s statewide mask mandate is lifted. The governor clarified that while the broader mask mandate will lift however masks will still be required in schools and for large gatherings.
April 16th: New Hampshire mask mandate is lifted.
May 3rd: Florida suspends all local Covid-19 emergency powers and issues an executive order to outlaw all local Covid-19 emergency mandates in the state effective July 1st.
May 12th: MGM Resorts’ Las Vegas Strip casinos approved for 100% capacity and no social distancing restrictions.
May 14th: Minnesota lifts mask mandate and leave businesses free to make their own decisions about whether to ask customers or employees to mask up. The Governor said that the time has come to discontinue the mask mandate that has stood since July 25th.
May 14th: Kentucky mask mandate is lifted.
June 10th: In Chicago 35,112 (including Bill Murray) people attend the first baseball game the venue has hosted since 2019.
May 14th: Pennsylvania mask mandate is lifted.
May 14th: Washington mask mandate is lifted.
May 14th: Illinois mask mandate is lifted.
May14th: Virginia mask mandate is lifted.
May 14th: North Carolina lifts indoor mask mandate.
May 15th: Maryland mask mandate is lifted.
May 19th: New York mask mandate is lifted.
May 19th: Connecticut mask mandate is lifted.
May 21st: Oregon mask mandate is lifted.
May 20th: The Governor of Iowa signs a bill into law that bans school officials and local jurisdictions from implementing mask mandates.
May 21st: Nevada mask mandate is lifted.
May 21st: The Governor of Texas issues an executive order that local governments or officials in Texas - including counties, cities, school districts and public health authorities - could no longer require the use of masks and face a fine of up to $1,000 for government entities or officials who continue to require mask wearing.
May 24th: Maine mask mandate is lifted.
May 29th: Massachusetts mask mandate is lifted.
June 7th: Texas bans businesses from requiring vaccine passports.
June 7th: The first live music festival since the March 2020 restrictions went ahead in Florida, for a three-day event where 22,000 people attended with no vaccine passports (they’re banned), no tests, no masks and no distancing.
June 15th: California lift most of state’s mask mandate except for large indoor gatherings, and there would be ‘no mandates and no restrictions in businesses large and small’.
June 30th: France lifts their mask mandate and end curfew.
July 15th: Indoor mask mandates are back in L.A. County regardless of vaccination status.
July 19th: ‘Freedom Day’ finally arrives in the UK and despite the name, many rules remain. Masks are no longer mandated but the Government has issued ‘strong guidance’ which states they are ‘expected and recommended’ in crowded spaces. Many airlines have made them a requirement for entry and the Transport Secretary Grant Shapps says he ‘expected’ operators to put in place ‘conditions of carriage’ to ensure that passengers were safe on public transport. There’s no indication if or when mask wearing will be repealed for good.
Options for increasing adherence to social distancing measures
The message is now clear - a reasonable and law abiding citizen wears a mask because it's the right thing to do and there's nothing wrong with following orders because everyone else is.
On March 22nd the UK government’s Scientific Advisory Group for Emergencies (SAGE) outlined the ways in which the UK population would need to be primed to accept the restrictions of civil liberty and personal freedom that would result from lockdown. These measures include persuasion, incentivisation and coercion. As is so often the case, when there is a choice between using the carrot or the stick, Government’s often fall back on one of their favourite tools: penalty fines.
One of the most powerful emotions we feel is exclusion and expulsion; in our tribal hunter-gatherer brain this equates to certain death. It can feel unbearable to not fit in and the use of shame has been a wonderful tool to get people to follow along with others for many centuries – 2020 is no different.
If someone told you last year the police would set up a hotline so people can report fellow citizens not wearing face masks, would you believe me?
That’s what police in Cuyahoga County, Ohio have done this month.
SAGE recommended various measures on how to establish compliance through methods of persuasion:
Perceived threat:
A substantial number of people still do not feel sufficiently personally threatened; it could be that they are reassured by the low death rate in their demographic group, although levels of concern may be rising...The perceived level of personal threat needs to be increased among those who are complacent, using hard-hitting emotional messaging. To be effective this must also empower people by making clear the actions they can take to reduce the threat.
Responsibility to others:
There seems to be insufficient understanding of, or feelings of responsibility about, people’s role in transmitting the infection to others...Messaging needs to emphasise and explain the duty to protect others.
Tailoring:
Some people will be more persuaded by appeals to play by the rules, some by duty to the community, and some to personal risk. All these different approaches are needed.
“It is hard to imagine a more stupid or more dangerous way of making decisions than by putting those decisions in the hands of people who pay no price for being wrong.”
Conclusion
With the Government making mask-wearing mandatory on public transport and retail assistants now wearing them in shops with no end-date in sight, it’s important to recognise there will be unintended consequences. The Government has ignored scientific evidence, not followed the precautionary principle and have enacted policies that have a hypothetical potential to cause harm. They claim they are ‘following the science’ but this implies there is consensus and, from the studies I’ve included, it’s clear that’s not true; you can cherry pick ‘the science’ to back up whatever narrative you want to fit it to.
The corporate media cannot be considered a trusted source of information for people wanting to learn more about the risks of wearing masks as they have consistently shown themselves to be sensationalists turning fact-based issues into ethical arguments and using fear and anxiety instead of data and education. They continue to broadcast and publish alarmist, unscientific, non-factual arguments in place of any research, statistics or peer-reviewed papers as well as censor professionals who don’t support their narrative. Important updates have been downplayed such as:
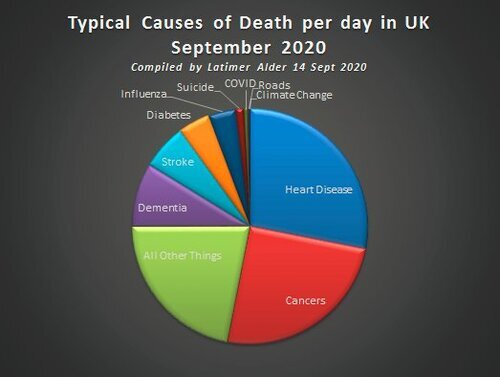
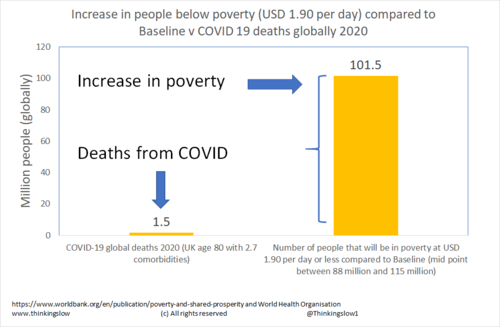
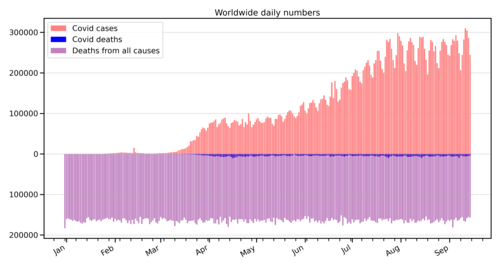
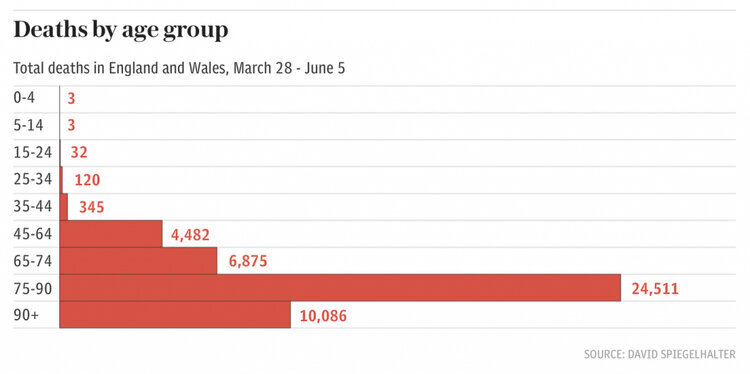
On 19th March the Government declared that Covid-19 is no longer considered to be a high consequence infectious disease in the UK.
The WHO declaring that asymptomatic transmission is ‘very rare’.
The latest immunological and serological studies which indicate the overall lethality of Covid-19 is about 0.1% meaning it falls in the range of a strong seasonal influenza.
If you choose to wear a mask, understand that the effect may not be neutral and there is a chance it can cause you harm because no medical intervention comes with a zero risk. A homemade cloth mask is more symbolic than it is functional; it provides the impression of safety and also helps us identify, judge and penalise those who aren’t wearing them. Aside from the health effects of mask wearing, we don’t yet know the psychological effects of wearing a mask on the individual and society. Wearing a mask is dehumanising; it is harder to hear people talking or read their emotional facial cues; this erosion of human contact may contribute to the loneliness epidemic which has very real health implications. Our feelings are not guideposts on how to act; they tell us nothing about what is right and wrong. We cannot live ethical, morally driven lives if we live under the dictates of emotions because emotions themselves are so easy to manipulate as the SAGE document shows.
No interventions such as masks or vaccines can come close to the importance of healthy living and developing your immune system so that you are less susceptible to infection and disease in the first place.
“For a Government to say we are so stupid and untrustworthy we will take this decision-making out of your hands is not acceptable in a democratic society. If you want a risk-free environment then you can lock yourself up. That’s a better alternative than the Government locking everyone up.”
Update
From July 24th (until when? the end of time?) face masks and coverings will be compulsory in shops in England. Aside from the economic impact of people choosing to shop online, thereby further decimating what’s left of the high-street, many people will only shop for essentials seeing as shopping has become so unpleasant. This is particularly ironic considering the Government advice published on the 11th May, and updated on the 9th July (just four days before the face-masks announcement), notes that ‘it is important to know that the evidence of the benefit of using a face covering to protect others is weak and the effect is likely to be small’. This was then updated on 23rd July to remove this statement.
The requirement to wear a face-covering does not apply if you have a reasonable excuse not to. Reasonable excuses include:
If putting on, wearing or removing a face covering would cause you severe distress.
If you have a physical or mental illness or impairment, or a disability that means you cannot put on, wear or remove a face covering.
If you are travelling with or providing assistance to, someone who relies on lip-reading to communicate.
If you are travelling to avoid injury or escape the risk of harm, and you do not have a face-covering with you.
If you need to remove it during your journey to avoid harm or injury or the risk of harm or injury to yourself or others.
If you need to eat, drink, or take medication you can remove your face covering.
If you are asked to remove your face covering by a police officer or other official, for example, to check your railcard.
The requirement to wear a face-covering does not apply to:
A child under the age of 11.
An employee of the transport operator, when they are acting in the course of their employment.
Any other person providing services to the transport operator, under arrangements made with the transport operator, who is providing those services.
A constable or police community support officer acting in the course of their duty.
An emergency responder such as a paramedic or fire officer acting in the course of their duty.
An official, for example, a border force officer, acting in the course of their duties.
If you are allocated a cabin, berth or other similar accommodation, at any time when you are in that accommodation, either alone, or only with members of your own household or a linked household.
If you are on board public transport but remain in your private vehicle, for example on a car ferry.
Please check the Government website for up-to-date information as this page isn’t updated regularly.
“By all means people can wear masks but they can’t say it’s an evidence-based decision… there is a real separation between an evidence-based decision and the opaque term that ‘we are being led by the science’, which isn’t the evidence.”
Mandatory mask-wearing discriminates against the disabled
Any businesses or staff who challenge people who are not wearing a face mask may end up dealing with someone who has a disability and, depending on how the situation develops, they may find they have committed:
an offence for which they are liable on summary conviction to pay a fine of up to £5,000 - section 112 (Aiding contraventions) of the Equality Act 2010; and/or
an act of disability discrimination and be ordered to pay to any individual who suffers injury to feelings compensation between £900 and £9,000 - section 119 (Remedies) of the Equality Act 2010.
Mandating everyone to wear masks discriminates against those with hearing impairments, and also people with phobias and mental health issues such as stress and anxiety, whether these have been clinically diagnosed or not. Some shops have already declared they will refuse entry or to serve customers who are not wearing masks unless the person presents an exemption letter from their doctor. That is confidential and sensitive medical information that should be private and secure; having to explain things to strangers and potentially show sensitive data is questionably illegal, plus it is both humiliating and distressing. Doctors letter requests – according to the GDPA such information is private and sensitive information and so enhanced GDPA requirements apply to requesting and supplying such data.
Why should anyone have to try and justify an exemption repeatedly and publicly to others whenever they shop?
People with hearing impairments are prevented from communicating with people who wear masks. This excludes them from communication they would otherwise engage in (i.e. using facial expressions and/or lip reading) and also removes their independence because they would need to be accompanied by someone without such an impairment who could translate for them by either removing their own mask to do so, or could use sign language.
People with hidden disabilities who come under the list of exemptions, should not face the embarrassment, humiliation or awkwardness of repeatedly explaining to strangers why they are exempt and justify why they are not wearing a mask. Under the DDA this in itself is discriminatory – i.e. a question of perception by the disabled person themselves, which makes them out to be publicly different from others and having to describe or show sensitive personal data which is normally classed as private and should be held secure.
Those people with hidden disabilities will now be made even more obvious and face discrimination from others because they are not masked – they face public challenges, refusals of service, harassment, social blacklisting, possibly legal challenges if police are called or they are spotted by a police officer, some will (and have already experienced this on public transport) attract threats and hate crime from those who do not understand the issues, or the disease transmission, or who have heightened fear for their own safety.
The above information was written by a Disability Rights campaigner.
“You may be 38 years old, as I happen to be. And one day, some great opportunity stands before you and calls you to stand up for some great principle, some great issue, some great cause. And you refuse to do it because you are afraid…. You refuse to do it because you want to live longer…. You’re afraid that you will lose your job, or you are afraid that you will be criticized or that you will lose your popularity, or you’re afraid that somebody will stab you, or shoot at you or bomb your house; so you refuse to take the stand.
Well, you may go on and live until you are 90, but you’re just as dead at 38 as you would be at 90. And the cessation of breathing in your life is but the belated announcement of an earlier death of the spirit.”

































![Screenshot_2020-07-14 face covering exemption card v3 proof - face-covering-exemption-extra-help-travel-assistance-card-12-[...].png](https://images.squarespace-cdn.com/content/v1/5a7989439f07f5f97873172d/1594726764782-79H1JJDE6IX33WWG0JRZ/Screenshot_2020-07-14+face+covering+exemption+card+v3+proof+-+face-covering-exemption-extra-help-travel-assistance-card-12-%5B...%5D.png)




























What are the most common misconceptions about furniture free? Well these are my top three!