Protect The NHS | At All Costs?
It's now week 10 of a 3 week lockdown and the NHS has been front and centre in peoples’ minds these last few weeks and close to many Brits hearts; ranking consistently at the of polls of what makes us proud to be British. Free at the point of use, the NHS is the crowning glory of the British Welfare State, created in 1948 and the first Universal Free Healthcare system in the world. This achievement was a signal of a fair and equal future for all of us and the NHS is, we are told, the envy of the world. It’s difficult to imagine how a country ranked 16th out of 35 countries in 2018 for healthcare - behind the Czech Republic, Estonia and Austria- would be looked on with such envy by citizens of other countries with far better health outcomes than ours, yet such a ridiculous idea persists in the British imagination.
Some describe it as the religion of the state; however the uncomfortable truth is that when you look under the surface, the NHS is being hollowed out from the inside to become a private healthcare system - modelled on the appalling American one. Funding the NHS to provide what is needed, where it’s needed, is no longer the prime objective. What we don’t have anymore is the NHS as a unified provider of universal and comprehensive services - between 7% and 22% of the healthcare budget already going to private providers.
The NHS is the closest thing the English people have to a religion.
Nigel Lawson, Chancellor of the Exchequer (1983 – 1989)
The decision to create a healthcare system that bears only an invisible cost to patients has meant they perceive it as entirely free. One consequence of this system is that GP’s act as a primary gatekeeper - without referral from a GP, it is often impossible to gain higher courses of treatment (such as an appointment with a consultant) whereas in other countries it is possible to gain direct access to a specialist.
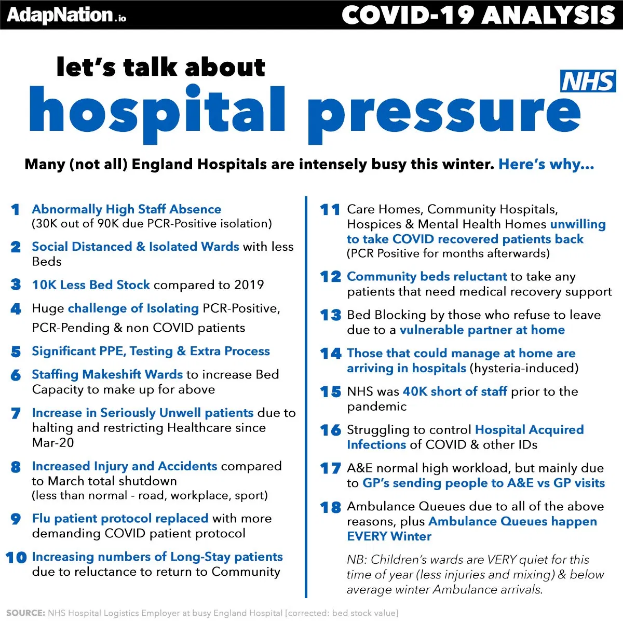
Fast forward to 2020 and the NHS has now taken on a mythical status, exemplified by the fact we’ve been experiencing the biggest mass quarantine in history under the guise of ‘Protecting the NHS’ - and have willingly submitted to it. Remember, the lockdown was presented as a temporary measure to spread coronavirus infections over a longer period to allow time for the NHS’s critical care capacity to catch up. It was never much of a rationale; the NHS is there to protect us, not the other way round.
We will eventually have to face up to the disastrous policy of sending highly infectious patients to district general hospitals and accept that in trying to save some lives we have condemned others to lose theirs.
‘As long as the hospitals themselves are reservoirs of infection, they will keep the epidemic going, re-seeding the community (together with the care homes). The lockdown, now renewed, is not necessary to protect the NHS. It is needed to protect us from the NHS. Until they sort out the hospitals and care homes, it will be unsafe to lift it.’
- Richard North
Germany has 38.7 ICU beds per 100,000 people, America has 29.4 and France has 11.6 - our ‘world-beating’ NHS has a measly 6.6 beds. How could its unpreparedness possibly justify depriving the entire country of liberty and freedom for who knows how long?
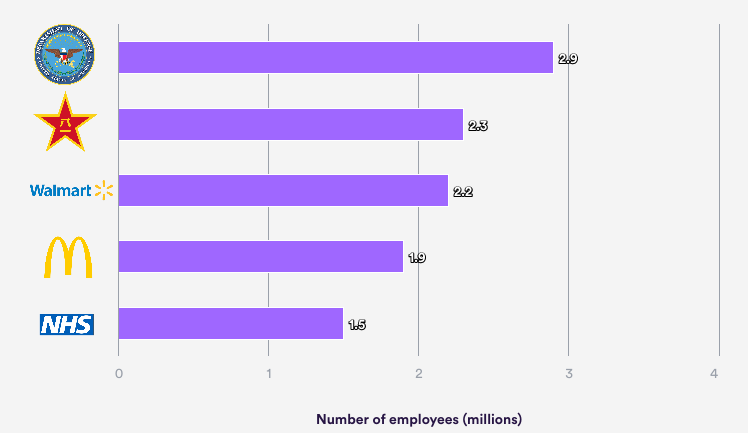
In 2020/21 the NHS has an operating budget of around £201.7 billion (which includes an additional £52bn of funding in 2020/21 for Covid-19) and, as of September 2020, it employs 1,313,765 people - 4.2% (53,012) more than in September 2019 (this is the figure for England, and does not include primary care staff). Professionally qualified clinical staff made up over half of the NHS Hospital and Community Health Service workforce (618,858) in September 2020.
Outsourcing
The NHS is broken up into over 500 ‘provider bodies’ which are a mixture of public companies called Foundation Trusts, the voluntary sector and private health. The Foundation Trusts aren’t under the direction of the Secretary of State for Health and act as legally independent organisations, set up in law under the Health and Social Care Act 2003.
They are able to:
- Set up their own subsidiary companies which may be either wholly owned or part owned with the private sector.
- Compete with each another alongside the private and voluntary sectors for contracts
- Sub-contract to the private sector for ‘extra capacity’
The first major shift towards privatisation began in the period between 1979 and 1997 when Conservative governments introduced GP Fundholding and compulsory competitive tendering for support services such as cleaning or catering. Ambulances, patient transport services, cleaning, maintenance and porters have also been outsourced to the private sector sometimes with serious consequences.
When a contract for a service is won by a private company, the NHS staff who had provided the service lose their employment with the NHS and there are no guarantees that the private company will retain the same pay and conditions staff had with the NHS. This leads to increasing fragmentation of the workforce and undermining their ability to bargain and negotiate rights and pay.
PFI and the NHS
The Private Finance Initiative (PFI) is a form of ‘partnership’ between the public and private sectors in which a group of private companies contracts to provide public facilities, often public buildings such as schools or hospitals. PFI has been used to build 127 hospitals and facilities which has also resulted in the NHS paying back these debts at very high interest rates.
It was first introduced by the Conservatives in 1992 and carried on after Labour came to power in 1997.
A PFI is like a mortgage that the government takes out on behalf of the public. The average annual cost of meeting the terms of the UK’s PFI contracts will be more than £10bn over the next decade.
And the cost of servicing PFIs is growing. In 2014 it rose by £5bn. It could rise further, with inflation. The upward creep is the price taxpayers’ pay for a financing system which allows private firms to profit from investing in infrastructure.
A case in point is Britain’s biggest health trust, Barts Health NHS Trust in London, which was placed in special measures in 2015. It is £93m in debt – struggling under the weight of a 43-year PFI contract under which it will pay back more than £7bn on contracts valued at a fraction of that sum (£1.1bn).
Unlike government funding, PFI’s cannot be adjusted to match the economy’s fortunes.
PFI was once hailed as the largest NHS hospital-building programme; in fact it is likely to end up becoming the largest hospital closure programme. Already PFI repayments have contributed to hospital mergers, closures and downgrades and Professor Allyson Pollock foresees these mergers being followed by the final “wave of closures in the run-up to privatisation and franchising out”.
Ideology At Our Own Risk
The roaring twenties that so many of us were hoping for have turned into a whimper, mere months after beginning. A cheery Bank of England forecast shows the UK is heading for its deepest recession in 300 years, with output plunging almost 30% in the first half of 2020.
We’ll have to wait and see how many furloughed jobs are still there waiting for people; 1 in 3 small firms that were forced to close due to the Government’s response to Covid-19 fear they’ll never reopen. The austerity measures we’ve lived under for a decade will undoubtedly have to continue, along with job losses and salary cuts. The main source of funding for the NHS is National Insurance contributions so this too will be affected by the fallout.
Planned spending for the Department of Health and Social Care in England is £140.4 billion in 2019/20 and 99% of this budget comes from taxes. So it’s clear the NHS cannot continue as it is and something will have to give; the vultures have been circling for years with stealth privatisation in the form of NHS ‘partnerships’ and the allocation of contracts to companies like Virgin.
For more information on this, watch John Pilger’s documentary ‘The Dirty War On The NHS’.
Free at the point of delivery is a held onto with an almost maniacal zeal, and it’s rare to find polls which show the general public will accept anything less than. However, just because it’s free at the point of delivery, doesn’t mean it’s free. A 2018 report conducted by The Institute for Fiscal Studies and The Health Foundation came to the conclusion that British households will need to pay an extra £2,000 a year in tax to ‘help the NHS cope with the demands of an ageing population’. Other forms of taxation have been put forwards including higher alcohol taxes.
The NHS is centralised and there is no competition to improve quality or compete for custom as there are no commercial pressures that shape it into being efficient and cost-effective. When salaries and pensions are guaranteed with or without an employees success you have a recipe for incompetence and wasted resources.
We’ve already seen pay freezes for the NHS workers and history has already shown that throwing money at the NHS hasn’t led to an improvement in care and outcomes. It is being hollowed out from the inside by a bloated middle management who have no training in health care but instead speak the language of money; this is the real profit before people. Doctors have been speaking out about the problems created by bureaucrats and the invisible managerial class who are paid handsomely, implementing policies and targets with little understanding of the real-world effects.
"The result is the perfect toxic professional working environment for this explosive mixture to generate disasters such as Mid Staffordshire which did so much harm to patients. Not even in Communist China did they have managers overruling doctors in the operation of hospitals and health services.”
- Dr Peter Holden at the British Medical Association’s annual conference in 2013
The Mid Staffordshire ‘disaster’ is a reference to the revelation that up to 1,200 people died unnecessarily between 2005 and 2009, left in complete squalor, some suffering from starvation or dehydration (patients resorted to drinking from vases because water couldn’t be left overnight due to ‘health and safety’).
Until I wrote this, I had no idea the extent the NHS was already privatised and moving towards the American model of healthcare by stealth - presumably due to the potential profits to be made rather than the poor healthcare outcomes. A country where 700,000 people are year are forced into bankruptcy to pay their medical bills warrants us sitting up and paying attention, lest that become us in the near future. Whenever other healthcare models are discussed in the UK, so often the response is, “well, I don’t want the American system”; however this isn’t an either / or situation; there are many different types of healthcare all around the world.
If we want to get the right answer, we need to ask the right question and we need to begin by asking what other healthcare systems are out there in the big wide world?
Which ones are successful in many different categories?
Simply parroting the emotive plea to ‘Save Our NHS’ has a nice ring to it but it simplifies the reality that things can’t continue as they are.
Now the NHS has transcended its original remit of providing free healthcare for all and become a symbol of a fair society, we are reluctant to let it go; we cling on to the idea of it out of faith instead of being clear-headed in searching for ways it can reform and improve to benefit us all. After all, the world in 2020 is very different than the one in which it was created in 1948. Something I’ve observed about the British is their sentimentality and nostalgia for the past; perhaps it’s a way to escape back to a time when Britain was ‘Great’ in the good ol’ days of Empire.
America
Healthcare is publicly and privately-funded through a patchwork of fragmented systems and programs. Insured Americans are covered by both public and private health insurance, with a majority covered by private insurance plans through their employers. The Affordable Care Act (also known as Obamacare) was introduced in 2010, yet 33 million people remain uninsured. Medicaid and Medicare are Government-funded and provide healthcare coverage to some vulnerable population groups.
America spends more public and private money combined on health care than any other OECD country yet despite being the most expensive system it is also is the worst-performing in terms of health access, efficiency, and equity. America consistently ranks low for infant mortality rate and life expectancy and those who are insured may be underinsured such that they cannot afford adequate medical care.
The price of pharmaceutical drugs is mind-boggling with an anti-allergic reaction device called an EpiPens costing $730 in 2016 despite containing about $1 worth of Epinephrine.
Germany
Germany has a universal multi-payer health care system paid for by a combination of statutory health insurance and private health insurance. Employers and their employees pay for most of the health care system in Germany through premiums. All workers contribute about 7.5% of their salary into a public health insurance pool. Employers match that 7.5% contribution. All Germans and legal residents of Germany are entitled to free 'medically necessary' public healthcare, which is funded by social security contributions.
Germany has long had the most restriction-free and consumer-oriented healthcare system in Europe. Patients are allowed to seek almost any type of care they wish whenever they want it. The governmental health system in Germany is currently keeping a record reserve of more than €18 billion which makes it one of the healthiest healthcare systems in the world.
This ‘all for one and one for all’ approach to health care has roots in the Middle Ages, when German craftsmen paid into one fund that was used to help any of its members in case someone became ill or suffered financial hardship.
Finland
Health services are available to all in Finland, regardless of their financial situation. Public health services are mainly financed from tax revenues; partly municipal, partly state tax. The system is highly decentralised and, although the Ministry of Social Affairs and Health has the highest decision-making authority, the municipalities (local governments) are responsible for providing healthcare to their residents. The prevention of diseases and other types of health promotion have been the main focus of Finnish healthcare policies for decades.
Switzerland
Switzerland combines private, subsidised private and public healthcare systems to provide its citizens with a large network of qualified doctors, best-equipped medical facilities and hospitals and no waiting lists. Healthcare is universal and health insurance is required for all people living in Switzerland.
Duties and responsibilities in the Swiss health care system are divided among the federal, cantonal, and municipal levels of government. The system can be considered highly decentralised, as the cantons play a critical role. Each of the 26 cantons (including six half-cantons) has its own constitution and is responsible for licensing providers, coordinating hospital services, and subsidising institutions and individual premiums. The federal government plays an important role in regulating the financing of the system, ensuring the quality and safety of pharmaceuticals and medical devices; overseeing public health initiatives; and promoting research and training. The municipalities, in turn, are responsible mainly for long-term care (nursing homes and home care services) and other social support services for vulnerable groups.
Luxembourg
The health service, overseen by Luxembourg's Union of Sickness Funds, ensures high quality, free and subsidised healthcare is available to all citizens and registered long-term residents. The state system covers the majority of treatments provided by GPs and specialists as well as laboratory tests, pregnancy, childbirth, rehabilitation, prescriptions and hospitalisation. The patient initially has to pay for the medical fees, which are decided on and revised annually by the Caisse de Maladie, and then submit the receipts for a reimbursement, which varies from 80 to 100%. Vulnerable groups are not obliged to pay any charges and students, unemployed and children are covered up until the age of 27. Although 99% of the population is covered by the state, private healthcare is also available and about 75% of the population purchases additional health insurance coverage.
Singapore
Healthcare in Singapore is supervised by the Ministry of Health. It largely consists of a government-run universal healthcare system with a significant private healthcare sector. In addition, financing of healthcare costs is done through a mixture of direct government subsidies, compulsory savings, national healthcare insurance and cost sharing.
Singapore has one of the most successful healthcare systems in the world both in health outcomes and finance efficiency, the success of which can be attributed to a combination of a strong reliance on medical savings accounts, cost sharing, and government regulation. The Government doesn’t directly regulate the costs of private medical care and keeps costs in check by regularly adjusting policies to ‘the supply and prices of healthcare services in the country’. Many people also have supplemental private health insurance for services not covered by the government's programmes.
Japan
Japan has offered full healthcare coverage for almost 60 years and is a hybrid system regulated by the government. It has three pillars of funding: government-managed plans, society-managed plans, and mutual aid associations with fees set by a government committee. All residents of Japan are required by the law to have health insurance coverage and depending on income and age, patients are responsible for paying 10%, 20%, or 30% of medical fees, with the government paying the remaining fee. Uninsured patients are responsible for paying 100% of their medical fees, but fees are waived for low-income households receiving a government subsidy. Patients are free to select physicians or facilities of their choice and cannot be denied coverage. Hospitals, by law, must be run as non-profit and be managed by physicians and medical fees are strictly regulated by the government to keep them affordable.
REFERENCES
Guest JF, Keating T, Gould D, et al, Modelling the annual NHS costs and outcomes attributable to healthcare-associated infections in England, BMJ Open 2020;10:e033367. doi: 10.1136/bmjopen-2019-033367
Sir Robert Francis, Freedom to Speak Up report
Report of the Mid Staffordshire NHS Foundation Trust public inquiry, 2013
Spending on the NHS in England
The sacred cow status of the NHS, BMJ 2015; 350 doi: https://doi.org/10.1136/bmj.h2651
£55 billion of NHS PFI debt has not been written off: with so much else that now needs to be reformed if the NHS is to serve us into the future
Crippling PFI deals leave Britain £222bn in debt
Overview of Health Management systems in the various countries cited
‘NHS is worse than communist China,’ say doctors
NHS needs £2,000 in tax from every household to stay afloat
Who pays the tab? The distributional effects of UK alcohol taxes, An Institute of Alcohol Studies report
The Spectator Covid-19 data tracker
How the Coronavirus Hoax Has Permanently Destroyed Health Care - Dr Vernon Coleman MB ChB DSc FRSA
NHS is free apart from the tax you pay and now it seems your freedom.
Blair SN, Physical inactivity: the biggest public health problem of the 21st century, British Journal of Sports Medicine 2009; 43:1-2.
40,600 people likely caught Covid while hospital inpatients in England
We patients protected the NHS – now its blaming us for its own failings















































What are the most common misconceptions about furniture free? Well these are my top three!